Introduction: Patients undergoing hip or knee arthroplasty (HA or KA) developed asymptomatic postoperative (post-op) venous thromboembolism (VTE) in around 30% of cases without any pharmacologic thromboprophylaxis (ThPPx). The use of pharmacological ThPPx after HA or KA has reduced the incidence of post-op VTE within 90 days to around 0.6-1.5%. People with bleeding disorders tend to have chronic joint damage from recurrent hemarthroses and frequently require HA or KA. This was especially true in the era before chronic factor prophylaxis. The exact risk estimate of post-op VTE in this population is unclear. Furthermore, the exact risk benefit for pharmacologic ThPPx is also unknown.
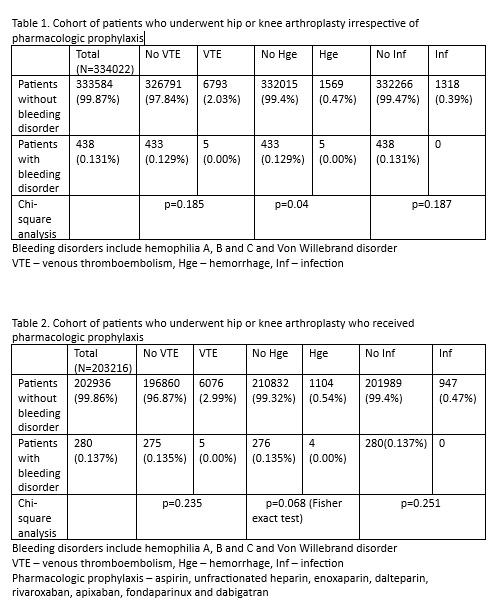
Methods: A retrospective cohort study was conducted by looking at patients who underwent HA or KA and stratifying them based upon whether they had bleeding disorder diagnosis. Data was collected from the Health Facts database, which contains de-identified information from the electronic medical records of all US hospitals in which Cerner© has a data use agreement. Patients with bleeding disorders included Hemophilia A, B, C and Von Willebrand disease. Incidence rates of post-op VTE, hemorrhage (Hge) and infection (Inf) were calculated and compared between patients with bleeding disorders and those without bleeding disorders regardless of pharmacologic ThPPx. The same outcomes were obtained and compared between patients with/without bleeding disorders who received ThPPx. Chi-square and Fischer exact test were used to determine statistical significance.
Results: 333,584 patients underwent HA or KA. Out of these, 438 patients had bleeding disorder. The incidence rates of post-op VTE were 0.01% in patients with bleeding disorders vs 0.02% in those without (p=0.1850) regardless of ThPPx which was not statistically significant. The incidence rate of post-op Hge was higher in patients with bleeding disorders (0.01%) compared to patients without bleeding disorder (0.004%; p=0.0404). The difference in incidence rate of Inf was not statistically significant between the two groups (p=0.1768). Out of total patients, 202,936 patients who underwent KA or HA received ThPPx. The difference in incidence rates of VTE as well as Inf were not statistically significant between patients with and without bleeding disorders who received ThPPx (p=0.2357 for VTE and p=0.2519 for Inf). The incidence rate of post-op Hge in patients who received ThPPX and had bleeding disorder was 0.014% in contrast to 0.004% in patients without bleeding disorder, though, it did not reach statistical significance (p=0.0684).
Conclusion: Patients with bleeding disorders have a similar risk of post-op VTE as the general population after HA or KA. Patients with bleeding disorders have higher post-op hemorrhagic complications. However, when comparing only those patients who received ThPPx, the difference in incidence of post-op Hge was not statistically significant. This implies that all patients including the ones with bleeding disorders, undergoing HA or KA may be treated with a similar ThPPx approach. Patients with bleeding disorders undergoing HA or KA do not have a higher predisposition to infections compared to the general population and may not require additional infection control measures. We did not look at the differences in factor treatment perioperatively which would have been standard for all bleeding disorder patients if they followed in a hemophilia treatment center. Our study limitation was its retrospective nature as well as all HA, KA, post-op VTE, Hge and Inf were identified by CPT and ICD codes.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal